Enhancing Gut Health: 9 Scientifically Supported
Strategies for Naturally Nurturing Your Gut
Microbiota
JUMP TO:
- The Benefits Of Good Gut Health
- Signs And Symptoms Of An Unhealthy Gut
- How Long It Actually Takes To Heal Your Gut
- 9 Science-Backed Habits To Improve Gut Health
- Best Foods For Gut Health
- Benefits Of Fiber
- Probiotics Versus Prebiotics, Explained
- Best Supplements For Gut Health
Have you ever experienced a stomach-in-knots kind of workweek or a series of not-so-solid (literally) bowel movements and thought, Could I have a gut issue? You’d be far from alone.
Yes, your gut health is important. But wellness fanatics, in many instances, have been making things waaay more complicated than they need to be when it comes to how to improve your gut health naturally.
What’s true is that researchers and medical professionals are continuing to find that strong gut health goes way beyond digestion. You’ve got an entire colony of microbes inside your body running the show. They do in fact affect how swollen or gassy you feel after eating, but they also have a hand in your immunity, heart health, mood, and more.
But working to improve your gut health isn’t necessarily the answer to every single health woe you have…and not everyone has a gut problem in the first place.
“As with everything else in health, I have to issue caution: There are hyperbolic, ridiculous claims on the Internet regarding the gut,” says board-certified internist and gastroenterologist Will Bulsiewicz, MD, author of The Fiber Fueled Cookbook. “It’s important to be careful about where we get information from and who you choose to trust.”
As it turns out, you can do most of your gut-health heavy lifting with some well-planned nutrition, sleep, and stress-management interventions that are essentially free of charge yet make a massive difference in how you feel on a daily basis. Consider this your no-BS guide.
Advantages of Optimal Gut Health
Gut microbiota refers to the colony of microorganisms, such as bacteria, fungi, and viruses, that live inside your intestines and stomach. It’s what makes you, well, you.
“Your microbiome is a part of who you are. It’s deeply personal and very unique to every single one of us,” says Dr. Bulsiewicz. “It is completely intertwined with your body’s physiology, and the way your biology functions is dependent on these microorganisms.”
The buzzy term gut health gets thrown around *a lot* and refers to the health of this community of microorganisms and the benefits to your well-being that you receive “in return for nurturing them,” Dr. Bulsiewicz says.
What’s more, your microbiome responds dynamically and dramatically to your diet and lifestyle. “The microbiome can produce chemicals that enter your bloodstream and spread throughout your body and brain. Because of their ability to do this, they can have an effect on so many aspects of your body and how it works,” Dr. Bulsiewicz says. An unhealthy gut can increase your risk for a host of diseases, including diabetes, heart and neurological diseases, allergies, and inflammatory bowel disease, according to the National Institute of Environmental Health Sciences.
Indications and Manifestations of an Imbalanced Gut
Recurring Episodes of Diarrhea or Constipation. We all have less-than-ideal bowel movements from time to time (like after that spicy meal). If it’s happening regularly and interfering with your day-to-day, that’s a sign to speak to your doctor.
Regular or Troublesome Bloating. Disorders such as irritable bowel syndrome (IBS), problems digesting certain carbohydrates, bacterial overgrowth in the small intestine, and other digestive diseases like chronic constipation and celiac disease can be behind that frequently bloated feeling, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Excessive Flatulence: Managing Excess Gas in the Digestive System. Most people pass gas eight to 14 times a day, but even up to 25 times is normal, according to the NIDDK. More frequent farts, or ones that come with extreme abdominal discomfort or pain, may be due to an overgrowth of or change in the bacteria in your small intestine, or the gut-related disorders mentioned above.
Unsettled Abdominal Sensations. Bloating and gassiness can both contribute to stomach pain. If you feel uncomfortable in your abdominal area long after eating, or when you didn’t just consume a meal, keep tabs on your symptoms to have a discussion with your doctor.
Indications in Different Body Regions. Non-GI clues such as fatigue, muscle and joint pain, skin rashes, brain fog, headaches, and mood problems may also result from something funky happening in your gut. “Poor gut health, also known as dysbiosis, or an imbalance of gut bacteria, can cause a variety of symptoms. How it presents varies from person to person, and the reason for that is unknown,” says Amy Burkhart, MD, RD.
A little perspective, though: “We all get bloated or have indigestion sometimes,” says Dr. Bulsiewicz. “It doesn’t mean that every time we’re bloated, we have a GI problem and need to be concerned.”
What is concerning is if any of the problems above are chronic, meaning they come and go for an extended period of time. “There are many definitions of a chronic condition, but in general, it is a condition that lasts three months or longer and may require active medical treatment or may limit activities of daily living,” says Dr. Burkhart. “If the symptom interferes with activities of daily living, especially on a recurring basis, it could be considered a chronic symptom.”
In addition, it’s really tough to self-diagnose. That’s where an evaluation from your doctor can differentiate normal from may-be-a-problem belly puffiness or gas, for instance. “When you think about these common digestive problems, if you look under the hood, you’ll discover the gut microbiome may be playing a central, but not exclusive, role,” Dr. Bulsiewicz says. The gut may not tell the whole story (and it may not be the entire solution).
If you’re having the more severe symptoms below, or noticing GI problems along with additional body-wide symptoms (joint pain, skin rashes, an uptick in headaches), then you should see a doctor.
The Timeframe Required for Gut Healing: What to Expect
Changing your gut health is a process. “It’s impossible to say ‘by so-and-so date, you’ll [feel] different,’” says Dr. Bulsiewicz.
That said, the gut microbiome can be altered pretty quickly. In fact, people who upped their fiber intake to 40 to 50 grams per day for two weeks had measurable changes in the composition of their gut microbiome; certain bacteria that ferment fiber, such as Bifidobacterium and Lactobacillus, were among the bacteria that grew more plentifully, per 2021 research in mSystems.
In Just One Month, Witness a Profound Transformation in Your Microbiome.
Make gut-supporting changes you can stick with for the long haul, Dr. Bulsiewicz recommends. “Within a month, you’ll start to have a dramatic shift in your microbiome. And if you sustain that habit, it’ll keep going,” he says. (Read: A small change you can maintain over time is better than any short-term cleanse or diet.)
9 Evidence-Based Practices for Enhancing Gut Health
Nutrition is arguably the largest piece of the puzzle, but it’s still “just one piece,” says Dr. Kwok. “Gut health is a series of small, intentional steps you take every day, week, and over the year that will guide you in the right direction.” Here’s how you can support belly balance:
Sleep well. ▸ Aim for seven to eight hours of sleep every eve. Poor sleep has been linked to disruptions in the gut microbiome in several studies, says Dr. Burkhart.
Go to bed earlier. ▸ “It’s not just how long you sleep, but the time you go to bed,” says Dr. Bulsiewicz. Just as your body runs on a circadian rhythm, so do your microbes. “They are sensitive to the time of day, just as much as we are,” he explains. This is your gentle nudge to stop the before-bed scroll one to two hours before you go to sleep. As for the ideal bedtime? Around 10 p.m. is a solid plan, but at the very least, try to close your eyes when you start to feel sleepy.
Fit in daily movement. ▸ “Regular exercise creates positive changes in the gut microbiome,” says Dr. Burkhart. Performing moderate to high-intensity exercise for 30 to 90 minutes at least three times per week for eight weeks was found to shift the microbiome in both healthy people and those who had health conditions, according to a new review of 28 studies in Nutrients.
Get active on your commute. ▸ People who spent time actively commuting—walking or cycling—had an increase in the richness and diversity of certain health-promoting microbes, found a recent study in PLOS One.
Manage stress. ▸ You know how when you’re stressed, you can feel it in your tummy? There’s evidence that stress changes the community of belly bugs, research suggests. Now’s the time to develop the stress-management strategies that really speak to you, whether it’s your favorite type of breathing (diaphragmatic or box, for example), reading, going out for a run, or spending time in nature.
Use antibiotics wisely. ▸ Antibiotics don’t kill only bad bacteria; they go after the good stuff too. That’s why they can reduce bacterial diversity and drive antibiotic-resistant infections, per Frontiers in Cellular and Infection Microbiology in 2020. Of course, there are many times when you need antibiotics. However, make sure you’re taking antibiotics only when you need them (e.g., for strep throat or a urinary tract infection) and not when you don’t (they are completely useless for colds, a sore throat, the flu, and many sinus infections), according to the Centers for Disease Control and Prevention. They won’t help you get better, and you’ll wipe out helpful bacteria in the process.
Fall in love with mocktails. ▸ Point blank: Limit or eliminate alcohol intake, as it’s a well-known gut irritant, says Dr. Burkhart. The best way to gauge whether you need to cut back for the sake of your gut is by checking in with yourself: Are you having GI issues, joint or muscle pain, problems sleeping, energy dips, or mood problems after drinking alcohol? Dr. Burkhart recommends nonalcoholic alternatives like all the fun new mocktails out there, such as Hiyo, Curious Elixirs, or (Katy Perry’s!) De Soi. “Many of the products also contain adaptogens that will lower stress, a common reason people reach for a glass,” she adds.
Get enough B12. ▸ Nutrient deficiencies affect microbiome health, says Dr. Burkhart, and one study found that B12 in particular (found in salmon, tuna, beef, yogurt, and fortified breakfast cereal) may be associated with bacterial diversity and abundance, according to a review last year in Advances in Nutrition. You’re at a higher risk for B12 inadequacy if you have a GI disorder or are vegetarian or vegan. If you have a limited diet, ask your doctor at your next appointment if you need to be tested.
Hydrate. ▸ “Dehydration leads to inflammation,” says Dr. Burkhart. In addition, people who drink high amounts of water (34 ounces of water daily) have a different bacterial makeup compared with those who drink low amounts, found a 2022 study in The Journal of Nutrition. Specifically, they had less of one type of bacteria associated with GI infections. In the end, it’s clear: What’s good for your gut is good for you too.
Top Nourishing Foods for Gut Health
If you generally feel good every day, a food-first approach already puts you on a great track to having a healthy gut. Let this nutrition rundown guide your next grocery haul…
“I advocate that patients eat a diet rich in fruits and vegetables, which promotes an equilibrium in the gut bacteria and has an anti-inflammatory effect,” says Dr. Kwok. Plant compounds called phytochemicals have been shown to boost beneficial bacteria, a recent review in the International Journal of Molecular Sciences found. Aim for 1.5 to 2 cups of fruit and two to three cups of veggies per day, the USDA recommends.
Many fruits and veggies are packed with fiber, but so are nuts, seeds, and whole grains. “Fiber feeds the good bacteria and helps balance the gut,” says Dr. Burkhart. (Save the handy infographics to come!)
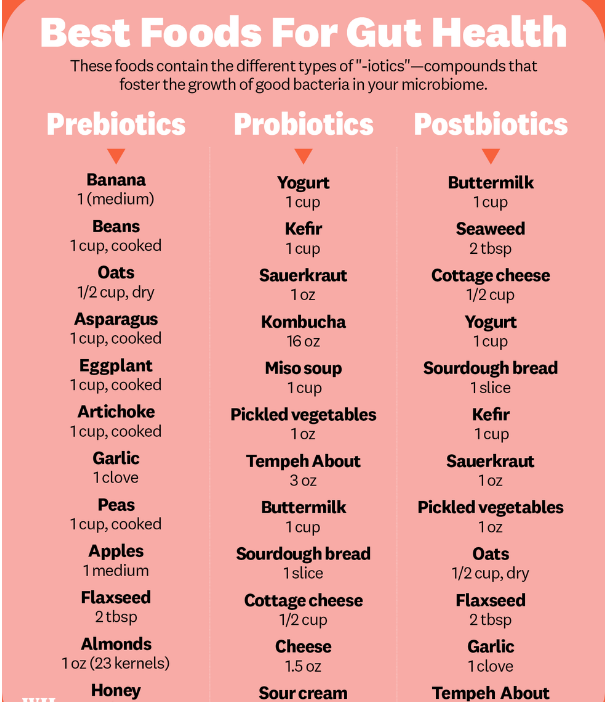
Foods such as miso soup, sauerkraut, kefir, kombucha, and Greek yogurt (peep the full -biotics food list ahead!) contain live active cultures that add beneficial bacteria to your microbiome. People who followed a diet high in fermented foods (slowly increasing to six servings per day) for 10 weeks improved gut bacteria diversity and decreased inflammation compared with those on a high-fiber diet, found a small study by Stanford University researchers.
Certain foods—like bananas, garlic, chickpeas and oats—are rich in a type of prebiotic fiber that helps feed “good” gut bacteria, says Dr. Kwok.
Postbiotics are the end products of probiotics and prebiotics that have health-promoting properties. These metabolites, too, can feed good gut bacteria, says Dr. Burkhart. Foods with postbiotics include buttermilk, seaweed, fermented foods, fiber-rich foods, and cottage cheese, she says.
A standard American diet is packed with ultraprocessed food, such as fast food and sugary bevs, which may promote inflammation and potentially alter gut microbiome diversity, says Dr. Kwok. No one’s asking you to totally give up your fave cookies—it's all about moderation. See if you can bring in more whole foods to see if that makes a difference in your digestive health. In the very least, the added fiber will probably help you poop more, leading to more day-to-day comfort. (TMI? Never!)
Benefits Of Fiber
Let us count the ways fiber is key for overall wellness: It’s good for your digestion, heart health, blood sugar control, and psychological health.
When it comes to your gut specifically, “fiber is the key source of nutrition for gut microbes,” says Dr. Bulsiewicz. Your intestines are a muscular tube that winds about 25 feet in your abdomen, the last five of which are home to the gut microbes. You need something to survive digestion and feed them—and that something is fiber, he notes.
Fiber perks up the composition, diversity, and richness of the microbiome. Different types of fiber are fermented in the gut by different bacteria. Therefore, filling up on fiber allows good bacteria to thrive and populate; and in general, the more diverse your microbiome, the healthier your gut.
Recos for fiber differ depending on age and sex. Females ages 19-30 should get 28 grams per day, females ages 31-50 should aim for 25 grams per day, and those over 51 years old should get 22 grams per day, according to the 2020–2025 Dietary Guidelines for Americans. Unfortunately, as many as 95 percent of Americans are not hitting their target, according to research in the American Journal of Lifestyle Medicine.
Soluble Vs. Insoluble Fiber
There are two main types of fiber: soluble and insoluble. “These are big umbrella terms. Under these two types, we don’t know how many types of fiber exist in nature,” says Dr. Bulsiewicz. “Each type has distinct and unique effects on the body.”
Soluble fiber dissolves, making a gel that slows digestion, according to the National Library of Medicine. Soluble fibers are fermented in the gut, promoting the growth and diversity of beneficial intestinal bacteria, per research in Molecules.
Insoluble fiber, on the other hand, is more difficult to digest, and so it bulks up your stool. (Think: the type of fiber found in roughage, like broccoli and the skin of apples.) Both types of fibers are necessary for a good gut, healthy poops, and also heart health.
Probiotics Versus Prebiotics, Explained
Probiotics are foods (or supplements) that contain beneficial strains of bacteria that can help populate your gut with the good guys. Prebiotics are also recognized as an important piece of the process. Prebiotic fibers in certain foods break down into food for the bacteria, so the bacteria can proliferate successfully.
The thing about probiotics is that different strains are used for different purposes. To better understand if you need one (or what you need), talk to your doctor first. However, if you’re looking into it ahead of your appointment, here are several options to chat with your health care provider about.
Probiotics are live microorganisms (also known as live active cultures) in fermented foods such as yogurt as well as in supplements, according to the National Center for Complementary and Integrative Health (NCCIH). Consuming probiotics stocks your gut with “good” bacteria.
Prebiotics are types of carbohydrates that make their way to your colon undigested, where your gut microbes feast on them. At that point, the party begins: They’re fermented by gut bacteria, a process that produces short-chain fatty acids, which have multiple perks, including lowering inflammation, supporting the immune system, protecting against cancer and diabetes, and helping to manage weight, according to recent research in Foods.
Best Supplements For Gut Health
If you absolutely know you can’t eat enough gut-supporting foods and are experiencing gut symptoms or have a chronic digestive disease, talk to a gastroenterologist about adding in a probiotic/prebiotic supplement.










0 Comments
Please do not enter any spam link in the comment box.